Prostate Surgery
Evaluation
Prostate
cancer continues to be the leading cancer in the
United States
male population. Surgical removal
remains the standard procedure for cure. Within the surgical arena, various
approaches for surgical extirpation have been employed. Currently there are
little objective parameters that are used to compare the efficiency of each form
of surgical removal. As surgeons apply these different surgical approaches, a
quality assessment would be most useful, not only with regard to overall
comparison of one approach vs. another but also with regard to a surgeonís
evaluation of personal surgical performance as they relate to a standard.
This research involves the development of a process employing image
reconstruction and analysis techniques to assess the volume and extent of
extracapsular soft tissue removed with the prostate by each of the various
surgical approaches. Parameters such as the percent of capsule covered by soft
tissue and where present the average depth of soft tissue coverage is assessed.
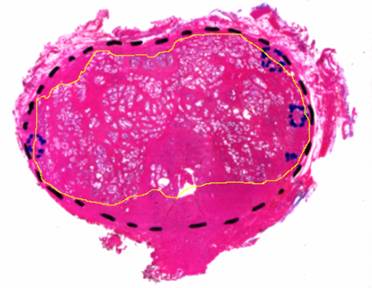
Below is a scanned image of a pathologically processed prostate slice showing
the boundary of the prostate gland capsule in yellow.
Figure 1: A prostate slice with the hand-drawn capsule
boundary
The research is performed at Old
Dominion University (ODU) and the Virginia Prostate Center (VPC) at Eastern
Virginia Medical School (EVMS). Using
preliminary (non-whole mount) data, ODU has investigated methodologies that can
be used to achieve statistically relevant results. EVMS, to date, has provided
preliminary data in the form of images from archived specimens. Additionally,
EVMS has obtained the necessary IRB approvals and has provided several
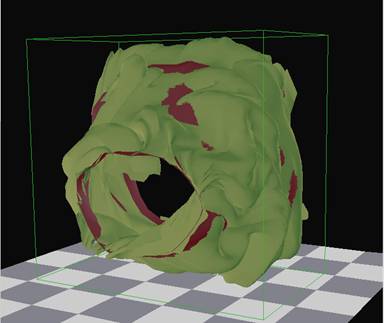
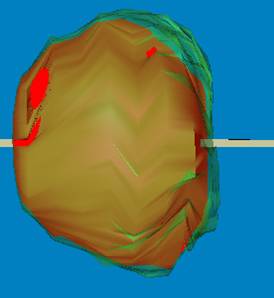
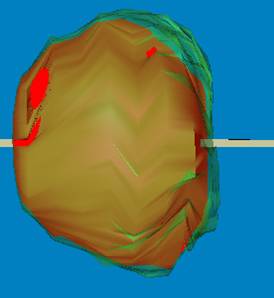
whole-mount prostate slices obtained from newly excised specimens. Figure 2 is
an example showing 3D reconstruction from these prostate slices.
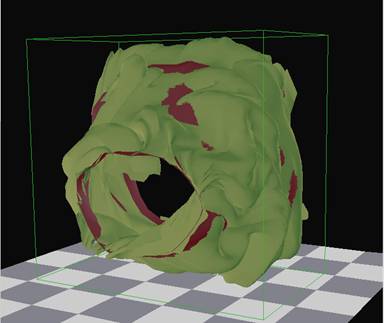
Figure 2:
Reconstructed 3D Model Showing Extracapsular Soft Tissue
A
final goal is to develop software for the purpose of a quality assessment for
pathologists and surgeons to evaluate the adequacy/appropriateness of each
surgical procedure; laparoscopic versus open perineal or retropubic
prostatectomy. This goal will be accomplished by evaluating readily available
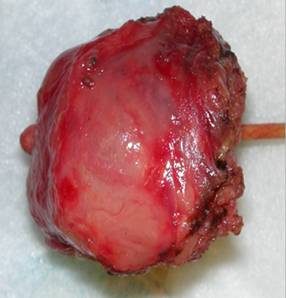
measurements. Figure 3 compares the fresh specimen with a 3D model showing the
bright red regions bare of extracapsular tissue.
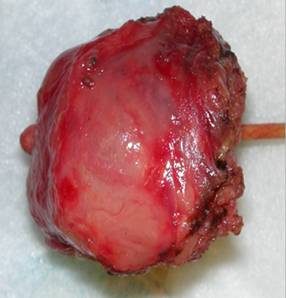
(a)
(b)
Figure 3:
Fresh prostate specimen (a) and reconstructed prostate model (b)
In
addition, software algorithms are being developed to perform automatic
recognition of the various determinant parameters and measurements leading to
the final assessment of quality assurance. These algorithms would include
automatic recognition of the prostate capsule and outer parenchymal contour.
Currently, this is tediously done by pathologists in order to facilitate
3D reconstruction of the prostate capsule and extra-capsular tissue.
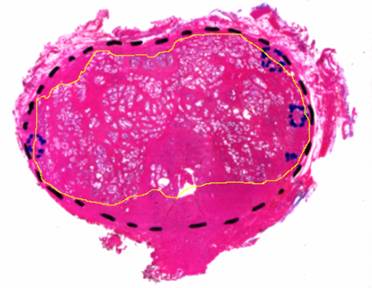
Figure 4: Prostate slice showing parenchymal contour in yellow
with prostate boundary in dashed black